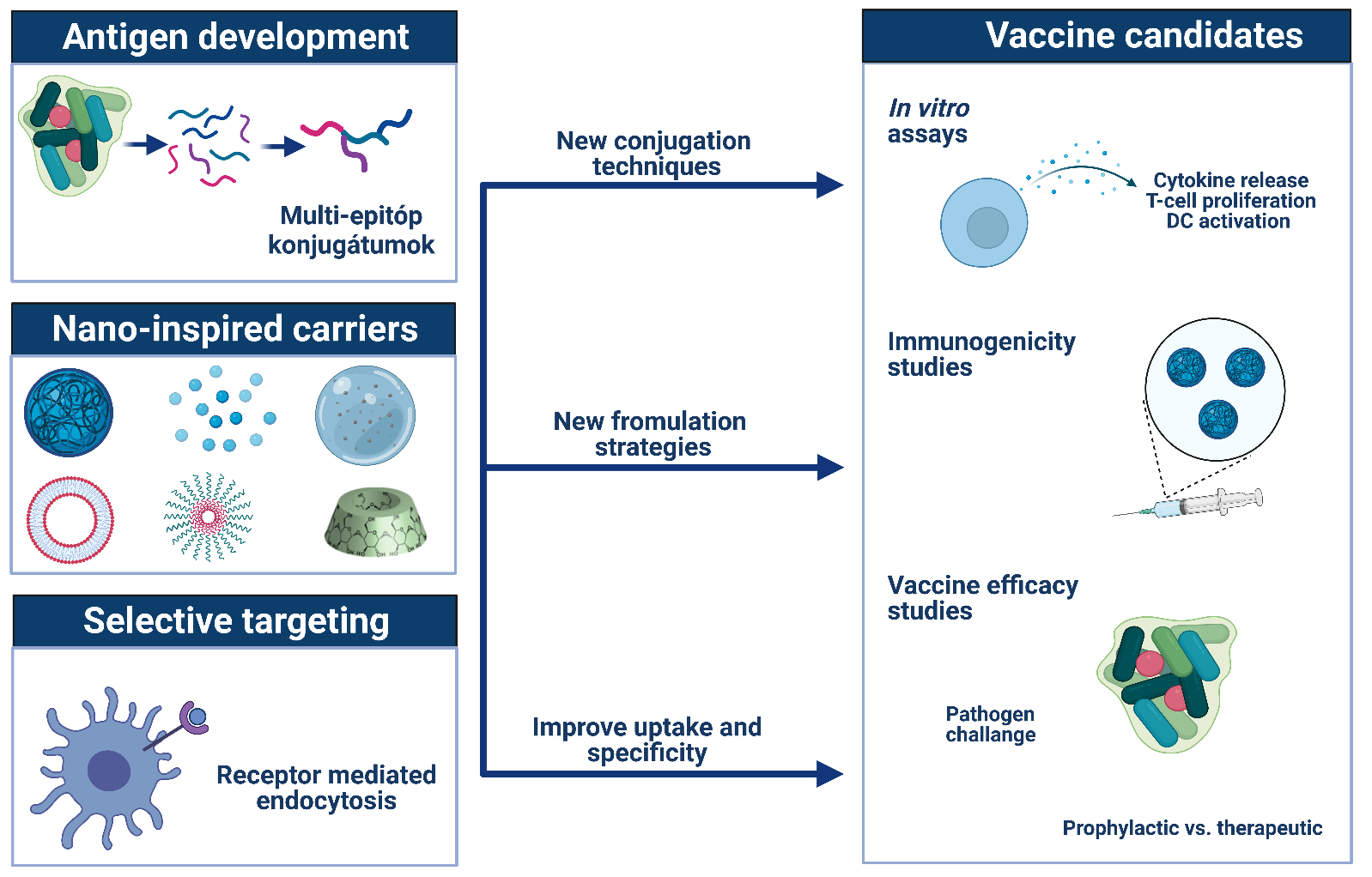
The Peptide-Based Vaccines Research Group was established in 2021 with the support of the MTA's Momentum Programme. The peptides, peptide derivatives and conjugates produced in the group are used in various research areas. New formulation strategies are being developed to enhance the biological activity of synthetic peptides and to maintain their stability. Using colloidal chemistry systems, we develop peptide delivery platforms with several advantageous properties such as target delivery, programmed drug release and enhanced immunogenicity.
Synthetic Vaccines
The prevention and treatment of a variety of infectious diseases, where the causative agent shows high antigenic diversity due to the metamorphosis across variation of stages or fast mutation rate, remains a major challenge today. Therefore, the development of vaccines with multiple immunodeterminants, instead of only one, is of great importance. In peptide-based vaccines, antigens of different origins can be combined to elicit a more general and effective immune response. However, subunit-type synthetic vaccines are generally not immunogenic enough on their own, the formulation used essentially determines the extent and quality of the immune response. Our research aim is to synthesise multi-epitope conjugates that can reflect on the variability of the pathogens and to develop new formulation strategies to increase the effectiveness of antigen presentation and overall vaccine efficacy.
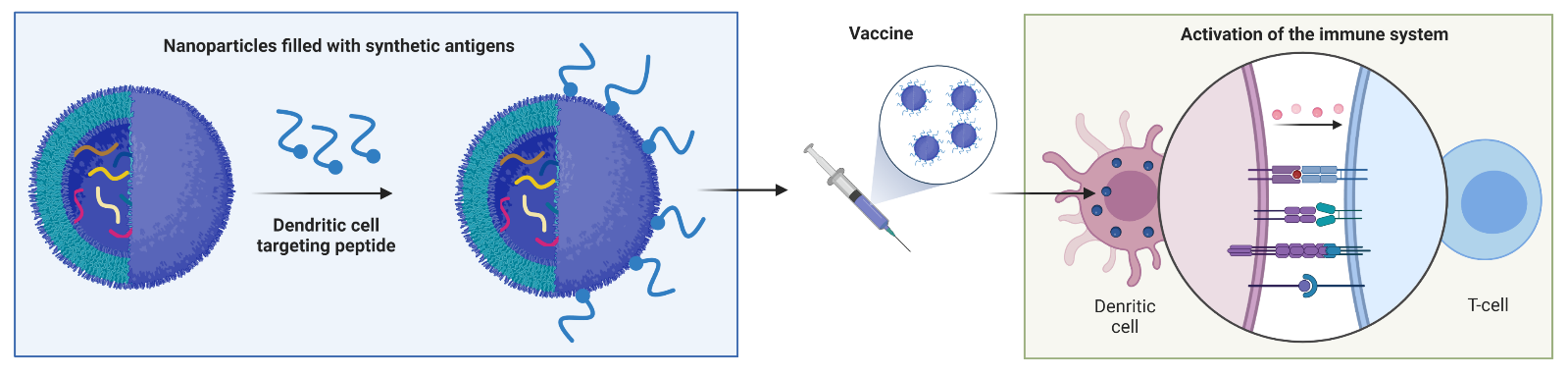
Dendritic cell targeting with peptides
Dendritic cells (DS) are professional antigen-presenting cells that play a key role in the generation of antigen-specific immune responses and immunological memory, as well as in the maintenance of immune tolerance. Treatment strategies based on targeting dendritic cells are therefore of great clinical relevance. In the present research we are developing synthetic peptides targeting cell surface structures and receptors of dendritic cells. Previously described DC-targeting peptides, that have been identified by phage display technology, are modified by peptide chemistry-based derivatization and structure-activity relationship studies are investigated with the aim of improving the targeting activity. The DC-targeting peptides are coupled onto the surface of multi-epitope vaccine conjugate-containing nanoparticels. The goal of this strategy is to improve the immunogenicity and overall efficacy of the vaccine constructs against chronic infections like tuberculosis.
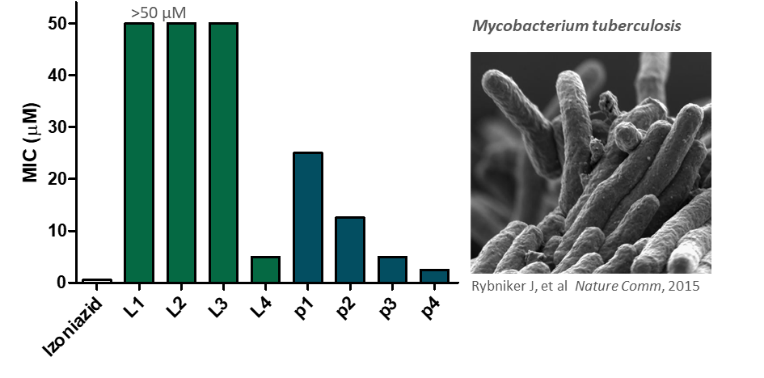
Antimicrobial peptides and peptide derivatives
We are mainly looking for compounds that are effective against bacteria that are resistant to conventional antibiotic therapies and therefore, difficult to eliminate. We are developing peptide-based agents against Mycobacterium tuberculosis and against the ESKAPE bacteria (Enterococcus faecium, Staphylococcus aureus, Klebsiella pneumoniae, Acinetobacter baumannii, Pseudomonas aeruginosa and Enterobacter sp.). By chemical modification of the peptides (e.g. fatty acid elongation) and the use of different delivery systems (e.g. PLGA nanoparticles, cyclodextrins), we aim to increase the antibacterial efficacy and selectivity of the compounds.
Synthetic vaccines for immunotherapy
Thanks to the rapid development of immunotherapy in recent years, it has become a mature treatment strategy. Immunotherapy has been used to achieve significant therapeutic success in a number of malignant tumours, with the activated immune system destroying tumour cells. Today, immunotherapy can be used alone or in combination with classical treatments. The immunotherapy has become more precise and personalised, with fewer side effects. Tumor vaccines aim to induce an immune response against tumor-specific or tumor antigens. Several of these are in clinical trials in breast, prostate and melanoma tumors, proving their viability in the field of tumor immunotherapy. The focus of our research is on melanoma, a highly aggressive, rapidly metastatic disease with high mortality. However, Melanoma accounts for only a few percent of all skin malignancies, it has the highest mortality rate. Before 2011, only chemotherapy and radiotherapy were used to treat metastatic melanoma, but their failure to improve survival has turned researchers' attention to immunotherapy. Dendritic cells have also pivotal role in the therapy of tumor diseases. Targeting dendritic cells is essential to induce an effect.
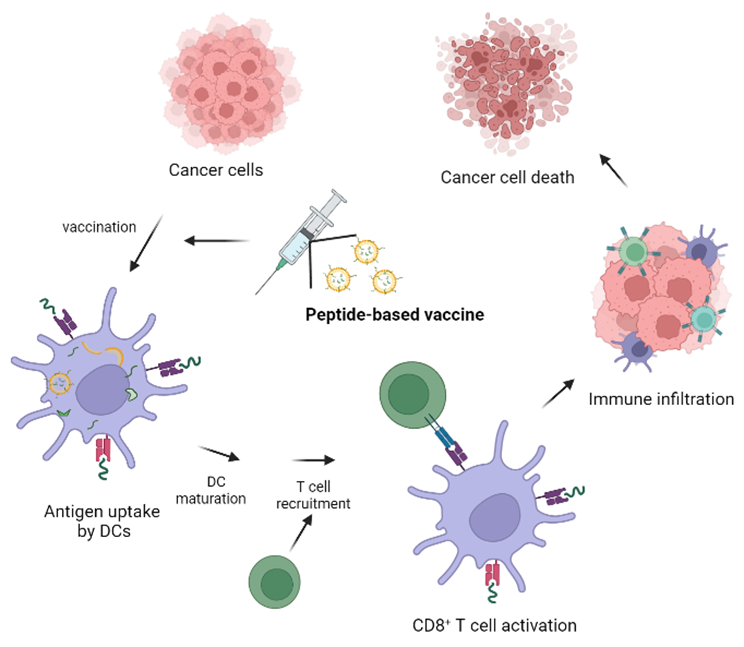
Melanoma-specific peptides and peptide derivatives
Based on the obtaine data from literature as well as from clinical trial, melanoma antigens are selected to be derived from epitope regions of both CD8+ T-cell (e.g., gp100 , tyrosinase, etc.) and CD4+ T-cell targeting proteins (e.g., MAGE-A3). By combination of these epitopes, chemical modifications (e.g. fatty acid conjugation) and appropriate selection of the carrier system, we can produce promising tumor vaccines.






